HCV Utility Pilot Study
Purpose
We have identified two important knowledge gaps in understanding the burden of Hepatitis C Virus (HCV):
- The utilities of Chronic Hepatitis C (CHC) patients who have late stage liver disease (decompensated cirrhosis (DC) and Hepatocellular Carcinoma (HCC)) are poorly understood.
- Most costs studies and utility studies have been conducted in tertiary care clinics. There are no studies on patients receiving care in the community.
We propose to measure the patient burden of HCV. This includes Health-related Quality of Life (HRQL) and health utilities in patients across CHC disease stages. It also includes the effect of HCV on workplace productivity, and costs borne by patients and families across different health care settings. This information will be useful for patients, doctors, and policy makers to make decisions on the new CHC treatments. Our results will have significant impacts on drug reimbursement policies and on guidelines for population screening.
Research Question
What are patients’ burdens of HCV, including HRQL and health utilities, across CHC disease stages?
Design and Methods
This is a multi-centre cross-sectional study, employing 7 self-reported questionnaires. The study cohorts will be selected from CHC-infected individuals attending tertiary care clinics or inpatient units of the University Health Network (UHN), or attending one of the 3 community clinics of the Toronto Community Hepatitis C Program (TCHCP) at Regent Park Community Health Centre, South Riverdale Community Health Centre and Sherbourne Health Centre. The tertiary care clinic patients are mostly middle class whereas most community clinic patients are from high-risk populations such as the homeless and intravenous drug users. We predict that their utilities will also differ.
Inclusion Criteria
Patients diagnosed with CHC without cirrhosis or HCC; or CHC with cirrhosis (compensated or decompensated); or CHC with HCC.
Exclusion Criteria
• Unable or unwilling to provide informed consent
• Psychiatric disorder impeding comprehension and completion of questionnaires
• Life expectancy of less than six months.
Progress
We have recruited 285 participants and have presented our preliminary findings in the 37th and the 38th Annual Meeting of the Society for Medical Decision Making and the 5th Canadian Symposium on Hepatitis C Virus. We are preparing the manuscript for publication.
Study Timeline
January 2015 – March 2017
Research Team
William Wong, PhD
Murray Krahn, MD, MSc, FRCPC
Karen Bremner, BSc
Julie Bruneau, MD, MSc
Jordan Feld, MD, MPH
Zeny Feng, PhD
Samuel Lee, MD
Kate Mason, MHSc
Nicholas Mitsakakis, MSc, PhD
Robert Myers, MD, FRCPC
Petros Pechlivanoglou, PhD
Jeff Powis, MD, FRCPC
Valeria Rac, MD, PhD
Josephine Wong, MD
Yasmin Saeed, PhD (Candidate)
Funding
CIHR Operating Grant
Publications / Presentations
Saeed Y, Mason K, Chung S, Altenberg J, Powis J, Bruneau J, Feld J, Feng Z, Mitsakakis N, Myers R, Rac V, Bremner K, Krahn M, Wong W. Health utilities in marginalized chronic hepatitis C patients participating in a community-based hepatitis C program. 37th Annual Meeting of the Society for Medical Decision Making, October 17-21, 2015. St. Louis, MO, USA.
SIESTA Study: Diagnosis of Obstructive Sleep Apnea with BresoDx®
Purpose
Research Questions
- How does the clinical diagnosis of OSA assisted by the home sleep study with BresoDx® in comparison with the clinical diagnosis assisted by the in-laboratory sleep study with PSG as the reference standard?
- What is the agreement between the AHI from the home sleep study with BresoDx® and the in-laboratory sleep study with PSG?
- What is the cost-effectiveness (cost per quality-adjusted life year) of the OSA after diagnosis based on home sleep study with BresoDx® in comparison with after diagnosis based on an in-laboratory sleep study with PSG?
Inclusion Criteria
-
Referral to a sleep clinic by a general practitioner or family physician with symptoms suggestive of OSA
-
Provide signed informed consent
-
At least 18 years of age
-
Ability to complete study questionnaires either on their own or with assistance
Exclusion Criteria
-
A history of chronic respiratory diseases (e.g., asthma, chronic obstructive pulmonary disease, lung cancer, cystic fibrosis and occupational lung diseases)
-
An existing diagnosis of other sleep disorders (e.g. periodic limb movement disorder)
-
A history of neuromuscular diseases (e.g., multiple sclerosis, muscular dystrophy)
-
A history of congestive heart failure
-
A history of stroke/Transient Ischemic Attack
-
Unable or unwilling to provide informed consent
Design and Methods
The SIESTA Home Sleep Study is a pragmatic, multi-centre randomized single-blinded two arm trial. This study focuses on subjects referred to a sleep clinic with symptoms suggestive of OSA. Study subjects will be randomized by a ratio of 1:1 to a sequence of home sleep study with the BresoDx® PM followed by an in-laboratory sleep study with PSG (the PM-PSG sequence) or the PSG-PM sequence. The target sample size is 250 subjects from 3-4 sleep clinics over a 4-5 month period evenly allocated between the two arms.
Study Timeline
Research Team
Funding
MaRS EXCITE
Publications/Presentations
Oral Presentations
2017 CADTH Symposium will be in Ottawa, Otario, from April 23, 2017 to April 25, 2017
Economic Evaluation of a Portable, Home-Testing Device (BresoDx) for Obstructive Sleep Apnea. Petros Pechlivanoglou
Diagnostic Accuracy of Level IV Portable Sleep Monitors Versus Polysomnography for Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. Lusine Abrahamyan
Mapping MFSAF and MPN-SAF to EQ-5D
Purpose
The purpose of this study is to develop a statistical model in order to map between Myelofibrosis (MF) specific Health Related Quality of Life instruments using the Myelofibrosis Symptom Assessment Form (MFSAF) and Myeloproliferative Neoplasm Symptom Assessment Form (MPN-SAF) and generic preference based utility instrument using EQ-5D. This will enable the estimation of utility values based on MFSAF and MPN-SAF data.
Research Questions
What is the mapping algorithm between two different types of instruments by using a simple linear regression method?
Inclusion Criteria
-
Patients with myelofibrosis from any English speaking countries including Canada, America, Australia, and England
-
Family members of myelofibrosis patients if patients are unable to participate the study by themselves
-
MF patients who can read, write, and speak English and complete the questionnaires
Exclusion Criteria
No specific exclusion criteria
Design and Methods
The study is composed of three parts: a) a systematic review of regression methods previously used for mapping, b) design and conduct of a survey of Myelofibrisis patients (including challenges arisen during the study), and c) the analysis of the survey data and mapping using statistical regression methods, which is the main part of the study. Patients with myelofibrosis from English-speaking countries will be asked to complete questionnaires which include both MFSAF/MPN-SAF and EQ-5D. Patients will be recruited through two ways: 1) online survey system using Survey Monkey or 2) direct mail out. Patients can choose the method to be participated.
Study Timeline
September 2013 - October 2015
Progress: Analyses are completed. A report was sent to Sanofi-Aventis Canada, the sponsor. Manuscripts are under preparation
Research Team
Chang-Ho Lee, BSc Honours
Funding
Sanofi - Aventis Canada, Inc.
Publications / Presentations
Lee CH, Bremner K, Grootendorst P, Ringash J, Krahn M, Mitsakakis N. Predicting utility scores for myelofibrosis patients: mapping the myelofibrosis symptom assessment form and myeloproliferative symptom assessment form to the EUROQOL-5D. 37th Annual Meeting of the Society for Medical Decision Making, October 17-21, 2015. St. Louis, MO, USA.
OSUN Study: Ontario Stroke Units
Purpose
Comparison of acute stroke care received at stroke units (SUs) to the care received in general medical wards (GWs) (i.e. care not received at SUs), specifically evaluating cost-effectiveness and characteristics associated with stroke unit care.
Research Questions
The primary research questions are:
- What are the characteristics of SUs in Ontario (i.e. frequently occurring, common characteristics)?
- Are SUs effective, as currently structured in Ontario?
- Are SUs cost-effective, as currently implemented in Ontario (i.e. what are the resources used and associated costs)?
- What SU characteristics are associated with improved patient- and system-level outcomes?
Design and Methods
The primary objective of the current research is to use a survey of hospitals in Ontario and data available from the Ontario Stroke Audit (OSA) to identify which specific characteristics of Ontario SUs appear to be (cost-) effective and are associated with improved patient outcomes, in comparison to GWs.
The characteristics of SUs in Ontario will be based on a telephone survey administered to all known SUs in Ontario. The comparative effectiveness and cost-effectiveness analyses will be based on the Ontario Stroke Audit (OSA) administrative database maintained by ICES.
Study Timeline
January 2013 - June 2016
Progress: Data collection started in January 2013.The final report has been completed and submitted to Ontario Stroke Network (OSN). The preparation of manuscripts is in progress.
Research Team
Murray Krahn, MD, MSc, FRCPC
Mark Bayley, MD, FRCPC
Moira Kapral, MD, Msc, FRCPC
Valeria E. Rac, MD, PhD
Luciano Ieraci, MSc
Gabrielle van der Velde, DC, PhD
Ruth Hall, BSc, MSc, PhD
Linda Kelloway, RN, MN, CNN(c)
Funding
Ontario Stroke Network (OSN)
Presentations/Publications
Rac VE, Sahakyan Y, Fan I, Luciano Ieraci, Ruth Hall, Linda Kelloway, Gabrielle van der Velde, Moira K. Kapral, Mark Bayley, Murray Krahn.The characteristics of stroke units in Ontario: a pan-provincial survey. BMC Health Services Research 2017 Feb;17:154. DOI 10.1186/s12913-017-2099-1
Sahakyan Y, Rac VE, Fan I, Ieraci L, Hall R, Kelloway L, van Velde G, Kapral MK, Bayley M, Krahn MD. Structure and function of stroke units in Ontario in 2013-2014. Presented at: Toronto General Research Institute (TGRI) Research Day, October 6, 2015; Toronto ON, Canada.
Ieraci L, Pechlivanoglou P, Bayley M, Kapral M, Fang J, Li S, Krahn M. Real-world effectiveness of stroke units in Ontario. A matched cohort analysis. Presented at: 2015 Canadian Association for Health Services and Policy Research (CAHSPR) Policy Forum; March 24, 2015; Toronto ON, Canada.
Rac VE, Sahakyan Y, Fan I, Ieraci L, Hall R, Kelloway L, van der Velde G, Kapral M, Bayley M, Krahn M. Structure and Function of Stroke Units in Ontario in 2013-2014. Poster session presented at: 2015 Canadian Association for Health Services and Policy Research (CAHSPR) Policy Forum; March 24, 2015; Toronto ON, Canada.
End of Life Care Interventions (EOL): Economic Analysis
Purpose
The annual cost of providing health care for patients in their last year of life is estimated to account for approximately 9% of the Ontario healthcare budget. Access to integrated and comprehensive pain and symptom management and comfort support for these patients appears to be inadequate and inequitable. We evaluated the cost-effectiveness of palliative care interventions to support policy development.
Research Question
What is the cost-effectiveness of evidence-based interventions for end-of-life care?
Inclusion Criteria
Not applicable.
Exclusion Criteria
Not applicable.
Design and Methods
Cost-effectiveness and cost-utility analyses from a health-care payer’s perspective. Target population: patients nearing end-of-life (according to observed population-based setting-specific patterns of palliative services) over the last year of life (one-year time horizon) and their primary informal caregivers. Comparators: “usual care” with current provision of palliative services in Ontario, “in-home” palliative team care (service provision either at home or long-term care), “in-patient” palliative team care, and “comprehensive” palliative care by a single team with care coordination across settings.
We included health care costs (2013 Canadian dollars; including home care, long-term care, hospital care, outpatient services, drugs, and physician billing costs), and additional costs of private insurance, out-of-pocket expenses, and time lost from paid work. Effectiveness measures were days at home, percentage dying at home (base case analysis), and quality-adjusted life days (QALD; sensitivity analysis).
We developed a state-transition microsimulation model to simulate palliative care needs by the target population. Model inputs were obtained from an end-of-life cohort of Ontarian decedents (n= 256,284) assembled from linked health administration databases (2007-2009), systematic reviews of randomized controlled trials evaluating palliative team care, and published literature. We conducted one-way and probabilistic sensitivity analyses.
Study Timeline
September 2014 – December 2014
Research Team
Ba' Pham, MSc, PhD
Robert Fowler, MD, MS, FRCPC
Peter Tanuseputro, MHSc, MD, CCFP, FRCPC
Doug Manuel, MD, MSc, FRCPC
Nancy Sikich, MSc
Shamara Baidoobonso, PhD
Petros Pechlivanoglou, MSc, PhD
Les Levin, MB, MD(Birm), FRCP(Lon), FRCPC
Murray Krahn, MD, MSc, FRCPC, on behalf of the Health Quality Ontario Expert Panel on End-of-Life Care, and the Toronto Health Economics and Technology Assessment Collaborative
Funding
Health Quality Ontario
Publications/Presentations
Ba' Pham, MSc, PhD (c), Robert A. Fowler, MD, MSc, Peter Tanuseputro, MD, MHSc, Douglas Manuel, MD, MSc, Nancy Sikich, MSc, Shamara Baidoobonso, MSc, PhD, Petros Pechlivanoglou, PhD, Les Levin, MD, MSc and Murray D. Krahn, MD, MSc. Cost-Effectiveness Analysis of Palliative Team Care for Patients Nearing End-Of-Life.Presented at: 36th Annual Meeting of the Society for Medical Decision Making; 2014 Oct 18 - 22; Miami, FL, USA.
Prognosis for Canadians Infected with HEP C, 1986-1990
Purpose
To estimate future treatment patterns with newly developed antiviral regiments for chronic hepatitis C (CHC) and update model predictions on long-term health outcomes in a Canadian hepatitis C compensation cohort.
Research Question
How will the newly developed antiviral regimens affect long-term health outcomes associated with compensation claimants with CHC?
Inclusion Criteria
Canadians who have been approved for compensation because of their acquired CHC during the period of 1986 to 1990.
Exclusion Criteria
Not applicable.
Design and Methods
A physician survey will be designed to understand the impact of new antiviral agent on treatment patterns with CHC who have similar background with the compensation cohort. A systematic review will be conducted to estimate their efficacies and toxicity by previous history of antiviral therapy and HIV co-infection. We will also maximize the use of the claim cohort data to estimate model variables and modify model structure according to the estimated future treatment patterns. Microsimulation will be run with the updated prognostic model to project lifetime risks of liver-related complications and mortality in current surviving compensation claimants. Sensitivity analyses will be also performed to explore the impact of model variable data sources, treatment pattern, and treatment uptake timeframe on model prediction.
Study Timeline
September 2013 - August 2014
Research Team
Murray Krahn, MD, MSc, FRCPC
Wendong Chen, MD, PhD
Qilong Yi, MD, PhD
William Wong, PhD
Funding
The 1986-1990 Hepatitis Settlement Trust Fund
Bayesian Regression Models for Disease-Specific Net Costs
Purpose
To estimate future treatment patterns with newly developed antiviral regiments for chronic hepatitis C (CHC) and update model predictions on long-term health outcomes in a Canadian hepatitis C compensation cohort.
Research Question
How will the newly developed antiviral regimens affect long-term health outcomes associated with compensation claimants with CHC?
Inclusion Criteria
Canadians who have been approved for compensation because of their acquired CHC during the period of 1986 to 1990.
Exclusion Criteria
Not applicable.
Design and Methods
A physician survey will be designed to understand the impact of new antiviral agent on treatment patterns with CHC who have similar background with the compensation cohort. A systematic review will be conducted to estimate their efficacies and toxicity by previous history of antiviral therapy and HIV co-infection. We will also maximize the use of the claim cohort data to estimate model variables and modify model structure according to the estimated future treatment patterns. Microsimulation will be run with the updated prognostic model to project lifetime risks of liver-related complications and mortality in current surviving compensation claimants. Sensitivity analyses will be also performed to explore the impact of model variable data sources, treatment pattern, and treatment uptake timeframe on model prediction.
Study Timeline
September 2013 - August 2014
Research Team
Murray Krahn, MD, MSc, FRCPC
Wendong Chen, MD, PhD
Qilong Yi, MD, PhD
William Wong, PhD
Funding
The 1986-1990 Hepatitis Settlement Trust Fund
EOL Care in Lung Cancer Patients in the USA and Canada
Purpose
To investigate the application of a novel statistical approach for the estimation of net costs attributed to a disease or health condition when only aggregate data are available and provided as collection of sample means and standard deviations for a number of strata. The proposed method is based on the application of a Bayesian Gamma mixed effects model, where both sample means and standard deviations are participating as stochastic nodes in the Bayesian model. The method is evaluated and compared with two simpler Bayesian Normal models using a series of simulation experiments.
Research Question
Does the proposed Bayesian Gamma mixed effects model offer an improvement for the estimation of net costs over simpler normal linear models, when only aggregate data are available?
Design and Methods
This is a study of development of statistical methods, using a series of simulation experiments.
Study Timeline
Oct 2010 – present (manuscript under revision)
Research Team
Nicholas Mitsakakis, MSc, PhD
George Tomlinson, MSc, PhD
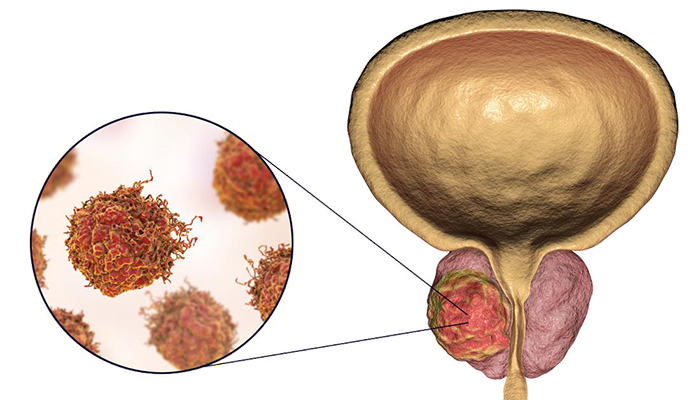
Androgen Deprivation Therapy in Prostate Cancer Patients
Purpose
To describe patterns of use, type and indication of androgen deprivation therapy (ADT) in prostate cancer patients in
Research Questions
- To determine the overall use and useof different types of ADT and its indications in the treatment of prostate cancer.
- To estimate costs for various types of ADT used for each indication.
- To estimate the incidence and costs of several of the most common side effects of ADT
Inclusion Criteria
The cohort will include Ontario Cancer Registry (OCR) patients assigned International Classification of Diseases-Oncology (ICD O) topography code C61.9 (cancer of the prostate) who had either bilateral orchiectomy or who received ADT pharmacotherapy for 3 consecutive months between January 1, 1995 and December 31, 2005, at age > 65.5 years, and who had no ADT therapy prior to January 1, 1995 or before age 65.5 years.
Exclusion Criteria
Exclusion critera are missing histology codes date of diagnosis the same as date of death, sex coded as female or missing, residence outside of
Design and Methods
Analyses will be conducted at the
Study Timeline
April 2007 to December 2013
Research Team
Murray Krahn, MD, MSc, FRCPC
Shabbir Alibhai, MD, MSc, FRCPC
Padraig Warde
Gary Naglie, MD, FRCPC
George Tomlinson, MSc, PhD
John Trachtenberg
Audrey Laporte, MA, PhD
Paul Ritvo
Karen Bremner, BSc
Funding
Canadian Cancer Society Research Institute
New Drug Innovation Fund (Ontario Ministry of Health and Long-term Care)
Beyond Case Fatality Rate
Purpose
To investigate potential methodological improvements in the estimation of the effect that uptake treatment increase of various treatments has on mortality as it is implemented in the IMPACT epidemiological model. The effect is measured by the number of deaths prevented or postponed. The method currently used in IMPACT model has data limitations, which could lead into biased estimates. This study proposes a probabilistic framework for the estimations in the IMPACT model, and presents how this framework allows naturally the application of the Potential Impact Fraction (PIF), a traditional epidemiological tool, for the estimation of the effect.
Research Questions
What is the magnitude of the bias introduced by the traditional methods of the IMPACT model in the estimation of the number of deaths prevented or postponed? Can the appropriate application of PIF reduce or eliminate this bias under different settings and assumptions?
Design and Methods
This is a study of development of statistical and epidemiological methods. It includes application of methods to real data originally presented in a previous study (IMPACT 2).
Study Timeline
Jan 2011 – present (manuscript published)
Research Team
Nicholas Mitsakakis, MSc, PhD
Harindra Wijeysundera, MD, FRCPC
Murray Krahn, MD, MSc, FRCPC
Economic Policy Model for HEP C
Purpose
To establish an economic model based on the best information available in the public domain on the natural history progression of hepatitis C to be used by Canadian Agency for Drugs and Technologies in Health (CADTH) to project long-term outcomes, costs and cost-effectiveness of interventions in treating hepatitis C to support clinical and reimbursement decision-making. The objective of this study is to build a flexible model platform that can evaluate the cost-effectiveness of CHC drugs and drug regimens that will be brought forward to the Common Drug Review for evaluation in the next few years.
Study Timeline
March, 2013 – September, 2013
Research Team
William Wong, PhD
Hong-Anh Tu, PhD
Wendong Chen, PhD
Jorden Feld, MD
Murray Krahn, MD, MSc, FRCPC
Funding
Canadian Agency for Drugs and Technologies in Health (CADTH)
Cost-effectiveness of Screening HEP C in Canada
Purpose
Chronic hepatitis C (CHC) is often asymptomatic and most individuals are not aware that they have been infected, thus the disease is often discovered when symptoms of late stage liver disease become apparent. In Canada, it is estimated that roughly 250,000, or almost 0.8% of the population, is infected with hepatitis C virus (HCV). Around 75% of those infected become chronically infected with the virus. 10-20% of whom will silently progress to cirrhosis and thereby be at risk of dying prematurely of liver failure and/or liver cancer. Early recognition of CHC probably extends the lifespan of infected individuals. Universal screening or screening for CHC among some high risk groups seems a plausible strategy. However, the potential health effects, costs, and cost-effectiveness of implementing a universal or selective hepatitis C screening program are unknown. The objective of this study is to build a model that can project the health and economic effects of various screening strategies for CHC conducted in different populations in Canada.
Study Timeline
July, 2013 – September, 2013
Research Team
William Wong, PhD
Hong-Anh Tu, PhD
Wendong Chen, PhD
Jorden Feld, MD
Murray Krahn, MD, MSc, FRCPC
Funding
Public Health Agency of Canada (PHAC)
CIHR-ICRH Estimating ROI of Circulatory Respiratory Health Research
As part of an international review, the Institute of Circulatory and Respiratory Health sought to determine the effects of research on the health of Canadians. Specifically, the Institute was interested in comparing the benefits obtained from funded cardiovascular-related research with the cost of that research in order to obtain an estimate of the return on investment.
The objective of this report was to estimate the return on public/charitable sector investment of cardiovascular-related research funded in Canada for the years 1975-2005. To do so, we performed a return on investment calculation closely based on the work of Buxton and colleagues, who estimated the return on investment of cardiovascular research in the UK. We also incorporated in our analysis an existing model, the Ontario IMPACT model, which characterizes changes in the burden of cardiovascular disease between 1995 and 2005 in Ontario, and determines the relative importance of specific risk factors and treatments. Wherever possible, we attempted to improve on the methods and approaches reported in previous analyses.
Our analysis involved several steps. First, we estimated the expenditures on cardiovascular research in Canada. Second, we estimated the health gains accrued in Canada between 1995 and 2005 from new cardiovascular treatments and procedures. This involved determining the number of unique users of these cardiovascular treatments and procedures, determining the quality adjusted life-years (QALYs) gained by each unique user identified above and the associated health care costs of these treatments, and determining the QALYs and associated health care costs from smoking cessation and potential smokers averted and monetizing the total number of QALYs. Third, we estimated the proportion of health gains attributable to cardiovascular research funded in Canada. Fourth, we estimated the time-lag between research expenditures realised and health gains obtained. Finally, we estimated the research and development spillovers from public sector investments. Once all the steps were performed, we were able to calculate the rate of return on investment and the internal rate of return.
Given our assumptions, we obtained an internal rate of return of 20.6% for research funded by the public/charitable sector. This means that every $1 invested in cardiovascular disease research in the public/charitable sector will yield a stream of benefits of roughly $0.21 to the economy per year, in perpetuity. If we consider a 12% hurdle rate as the minimum acceptable rate of return for a given investment, then our internal rate of return of 20.6% is very good. This suggests that Canadians obtain relatively high health gains for every dollar spent on cardiovascular disease research. When we added private cardiovascular disease-related research expenditures to the public/charitable ones and considered the impact of research spillovers, we obtained a combined social rate of return of 44% (12.9% + 31%).
Our analysis was based on previous work but also provided some improvements. In particular, our study improved methods for estimating the number of unique users in each patient group/intervention; considered differential treatment of health gains for individuals that quit smoking and for non- starters; estimated Canada’s contribution to global medical research; modelled the time lag between incurred research expenditure and realised health gains as a distribution, among others.
This work involved many assumptions. Accordingly, there were some areas of uncertainty. For example, it was unclear what proportion of health gains can legitimately be assigned to research. We also did not evaluate risk factors other than smoking and thus, our calculated value for the internal rate of return was probably an underestimate.
Nonetheless, this research will guide the Canadian Institutes of Health Research in determining the value of its current research portfolio for cardiovascular disease research. In addition, it will provide valuable experience in conducting this type of work in Canada, which can potentially be used in other aspects of the portfolio of the Canadian Institutes of Health Research, or by other granting agencies. Finally, this may represent an opportunity to collaborate with other countries in establishing and refining methods to document the value of medical research.
PUMTT Study
FIELD EVALUATION
Purpose
Research Questions
- Do EMDTs increase the rate of pressure ulcer healing, measured by wound surface area (cm2) over time (days), relative to Usual Care Teams (UCTs)?
-
Is the use of EMDTs to increase the rate of pressure ulcer healing cost-effective?
-
Are EMDTs more effective than UCTs in healing a greater proportion of pressure ulcers?
-
Are EMDTs more effective than UCTs in reducing the facility-acquired incidence rates of pressure ulcers?
-
Are EMDTs more effective than UCTs in reducing wound related pain and discomfort?
-
What are LTC facility staff perceptions and experiences associated with EMDTs for pressure ulcer management?
Facility Inclusion Criteria
-
must be located within the Toronto Central or Central LHIN geographic boundaries.
-
must have > 100 beds.
-
must be within 100 Km of the EMDT.
-
must be entering data into MDS.
-
must have a PU prevalence rate > the provincial average (5.5%) reported in the fourth quarter of 2009 MDS.
-
administrator must consent to participate.
Design and Methods
Study Timeline
Research Team
TURN Study
Inclusion Criteria:
-
Age 65 years or older and legally able to grant consent, or have an available surrogate who may legally grant consent.
-
At risk for pressure ulcer development with Braden Scale Scores of 10 to 14, indicating moderate (13-14) or high (10-12) risk.
-
Scores of 1 to 3 on the mobility subscale of the Braden Scale indicating some mobility limitations.
-
Expected to have a length of stay of 3 weeks for study participation.
-
Sleeping on a high density foam mattress
Exclusion Criteria:
-
Pressure ulcer(s) present on screening.
-
The resident cannot be turned on 3 anatomical surfaces (side, back, side) or has a contraindication to repositioning.
Research Team
WIT Study
Purpose
Research Question
Inclusion Criteria
-
Newly referred to Toronto Central Community Care Access Centre (CCAC) for wound management.
-
>18 years of age.
-
Client or Substitute Decision Maker (SDM) provides written informed consent.
-
Someone in the client’s home (or SDM) must be able to speak English.
Exclusion Criteria
-
Surgical wounds.
-
Burns.
-
Malignant wounds.
-
Clients deemed palliative.
Design and Methods
Study Timeline
Research Team
Funding
Health Quality Ontario